|
Sickle Cell Anemia: An Ardent Need for Awareness Development Along with Mass Screening
Barnali Chakraborty and Arup Majumder
Introduction
India is a great and vast country with diverse and multiple caste, ethnic group, religions, occupations, economic strata, languages, socio-cultural traditions, genetic heritages and life styles and practices. Moreover this country has absorbed in so many racial, religious, socio-cultural linguistics and genetic elements that have given rise to amalgamation, conglomeration of all the constituent features, representing the cohesive unity in diversity in true sense. Within these wide ranges of diversity, there exist mixed populations with various genetic disorders, which through time gradually dispersed throughout the country though not uniformly, but to some extent clustered in some population.
The occurrence of sickle cell gene in India was first reported by Lehman and Cutbush [17] among the Veddoids of Nilgiri hills. After that almost at the same time it was discovered in Assam among the tea garden laborers. India caters to nearly 20 million people with sickle cell diseases. Solanki and Shukla 29reported the first sickle cell case from Central India in the year 1958. Sickle cell anemia is an inherited disorder of hemoglobin synthesis. This happens due to replacement of valine for glutamic acid in position of 6 of the beta-globin chain of hemoglobin. The genetic alteration yields an unstable RBC with a shortened survival of 10-20 days instead of the normal of 120 days. Under stress, these irregular shaped red cells become rigid and sticky and die prematurely, resulting in a chronic shortage in the blood. While travelling through small blood vessel, they can get stuck and slow down or block blood flow. Sickle cells have relatively small oxygen contact area and increased blood viscosity and impaired normal circulation in small blood vessel, resulting in clots and infraction. In people with sickle cell anemia, these blockage produces pain and serious complications. These effects can however vary from person to person depending on the type of sickle cell disease, nutritional status and others concomitant factors.
The disease is found predominantly amongst certain high-risk communities belonging to schedule caste, schedule tribe and other backward classes Approximately 3.2 million population belongs to high risk communities in Central India. According to Kar 14 the sickle cell anemia gene is not confined to tribal peoples, but is prevalent throughout the society, being more frequent in scheduled caste and some other caste.
There is no treatment for complete cure of this inherited disease. The probable way to reduce this genetic disorder is to make people aware about these diseases, its pattern of inheritance and the possible risk factor by genetic counseling. Genetic counseling is the process by which patients or relatives, at risk of an inherited disorder, may aware about the consequences and nature of the disorder, the probability of developing or transmitting it, and the options open to them in management and family planning in order to prevent, avoid or eliminate it. This process involves appropriately trained persons to help the individual or family to (i) comprehend the medical facts, including the diagnosis, probable cause of the disorder, and the available management; (ii) appreciate the way heredity contributes to the disorder, and the risk of recurrence in specified relatives; (iii) understand the alternatives for dealing with the risk of occurrence; (iv) choose the course of action which seems to them appropriate in view of their risk, their family goals, and their ethical and religious standards, to act in accordance with that decision; and (v) to make the best possible adjustment to the disorder in an affected family member and/or the risk of recurrence of that disorder. Though the counselor discusses the risk factors associated with the ongoing conception in presence of both at-risk spouses, the decision regarding the available options depends solely on the attitude and acceptance of the individuals counseled (Fig: 1).
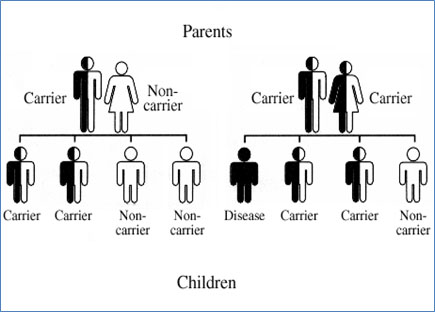
Fig. 1: Pattern of inheritance
Sickle cell disease (SCD) affects millions of people throughout the world and in particularly common among those whose ancestors come from Sub Saharan Africa, Spanish speaking people of Western hemisphere (South America, Carolinas and Central American, Sub Arabia, India and Mediterranean such as Turkey, Greece and Italy) (Fig: 2).
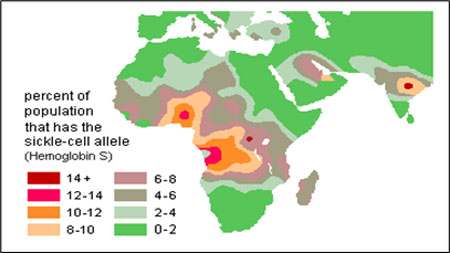
Fig. 2: Worldwide distribution of Sickle cell gene
With a large population, burgeoning birth rate, and consanguineous marriage practices, there is a dangerously high prevalence of genetic disorders among tribal populations. There remains a conspicuous lack of maternal and child health services among the tribal areas and consequently, the tribal demographic scenario is one of high fertility, high maternal and infant mortality rates. Epidemiological studies confirmed that sickle cell anemia is rampant in the tribal population (Association for Health Welfare, in the Nilgiris & Tribal India Health Foundation). Sickle Cell Disease Center, Operations report version 1.4. (www.tihf.org/scd.htm). Genetic diseases have received little attention from urban health services in India, and even less so in tribal areas. As a result, virtually all studies carried out regarding tribal populations and sickle cell disease have strongly recommended that genetic health services should be integrated into existing primary health care and medical services to combat the epidemic. Now, I try to give a brief description about the genetics of sickle cell and sickle cell gene in the following.
Genetics of Sickle Cell:Cells in tissues need a steady supply of oxygen to work well. Normally, hemoglobin in red blood cells takes up oxygen in the lungs and carries it to all the tissues of the body. Red blood cells that contain normal hemoglobin are disc shaped (like a doughnut without a hole). This shape allows the cells to be flexible so that they can move through large and small blood vessels to deliver oxygen. Sickle hemoglobin is not like normal hemoglobin. It can form stiff rods within the red cell, changing it into a crescent, or sickle shape. Sickle-shaped cells are not flexible and can stick to vessel walls, causing a blockage that slows or stops the flow of blood. When this happens, oxygen can’t reach nearby tissues. The lack of tissue oxygen can cause attacks of sudden, severe pain, called pain crises. This pain attack can occur without warning, and a person often needs to go to the hospital for effective treatment. Most children with SCD are pain free between painful crises, but adolescents and adults may also suffer with chronic ongoing pain. The red cell sickling and poor oxygen delivery can also cause organ damage. Over a lifetime, SCD can harm a person’s spleen, brain, eyes, lungs, liver, heart, kidneys, penis, joints, bones, or skin. Sickle cells can’t change shape easily, so they tend to burst apart or hemolysis. Normal red blood cells live about 90 to 120 days, but sickle cells last only 10 to 20 days. The body is always making new red blood cells to replace the old cells; however, in SCD the body may have trouble keeping up with how fast the cells are being destroyed. Because of this, the number of red blood cells is usually lower than normal. This condition, called anemia, can make a person have less energy (Fig:3).
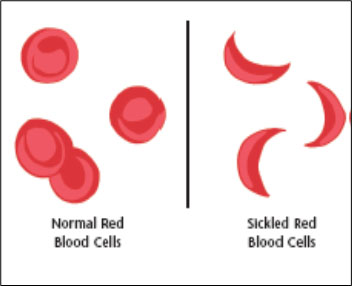
Fig. 3: Normal Red Blood Cells and Sickle Cells
About Sickle Cell Gene: There are a number of similarities between African and Indian as referred to certain type of sickle cell anemia especially in relation to the sickle cell gene common among Fulani. The Fulani people live painful crises, infections, acute chest syndrome is very harmful. The reason is mostly due to very high presence of alpha Thalassemia as well as high fetal hemoglobin levels. Throughout Africa. Linguist have reported that the Fulani and Dravidian languages are genetically related31, 32. Sickle cell anemia is named after the geographical region in which it is found. African tribal groups and Africans share Arab-India, Benin and Senegal sickle cell anemia1. The Senegal and Indian sickle cell share common haplotypes23.The Arab-Indian and Senegal haplotypes have same mutation at position 158,mainly found among the Indian tribal groups which have rarely interacted with outsiders makes it clear that it was probably carried to India when Dravidians migrated from Nubian (North Sudan) to South India32.It is interesting that the Arab-Indian and Senegal haplotypes are both associated with same mutation at position 158 of chromosome no 11 (eleven). Further conformations reveal that the African origin of the Dravidians because it is in the Senegal area where large number of Fulani population exist33.
The impact of sickle cell disease (HbS) among tribal population of India is generally similar in comparison to certain caste populations. In tribal population due to episode of painful condition is infections and acute chest syndrome is very harmful. Reason is due to very high presence of Alpha Thalassemia as well as high fetal hemoglobin level.
Besides having prominent cultural and behavioral uniqueness, the tribal of India also have their characteristic individuality with respect to their genetic make-up. Studies done on blood groups and immunity related genes have shown that tribal of India have sets of alleles which are exclusive to certain geographical area and ethnic groups3,5.The hypothesis that they differ distinctly in the pattern of distribution and frequency of specific sets of alleles from thenon-tribal Indian populations has been empirically proved by designed population based studies on hemoglobin apathies26,22. According to Indian Council of Medical Research(ICMR) survey Sickle Cell gene is found amongst different tribal groups of India (Fig.:1), which varies from 5 to 34 %28.
In Maharashtra, the sickle gene is widespread in all the eastern districts, also known as the Vidarbha region, in the Satpura ranges in the north and in some parts of Marathawada. The prevalence of sickle cell carriers in different tribes varies from 0 to 35 percent. The tribal groups with a high prevalence of HbS (20-35 %) include the communities of Bhils, Madias, Pawaras, Pardhans and Otkars. It has also been estimated that Gadchiroli, Chandrapur, Nagpur, Bhandara, Yoetmaland Nandurbar districts hosts more than 5000cases of sickle cell anemia 13.
Objectives
There is no treatment to cure this genetic disorder permanently only awareness is a compact process which begins with systematic input of knowledge about this genetic abnormality and further a consequent assessment of its impact in population. Unless a strong awareness concern is developed among the sickle cell carriers and disease person. The recurrent of these genetic disorders cannot be stopped or decrease in peculating among their siblings. Therefore, an effort has been made to educate people with this genetic disorder to understand the extent of this disorder and thereby developed a concern among them to cure the means of this disorder. The entire process of educating people about this disorder categorically broad under six distinct phases as Pre-Education Questionnaire, Post-Education Questionnaire, Follow- up Questionnaires Knowledge (Results of Knowledge Gain from Pre, Post, and 3 Month), Concern Result, Attitude result, Follow up (3 Month F/U-Education Questionnaire). The main objective of present study is to understand people only numbers of screening programs are not enough to change the scenario of sickle cell anemia. So, I may try to understand which type of awareness program is also necessary along with mass screening for these problems.
Methodology
The current study is framed under a vivid related literature survey, relating to sickle cell disease in India in general and Central India in particular. As per the current study it has become very clear that despite repeated attempt by different agencies to curve down the wild growth of sickle cell disease in India, the resultant outcome appears to be a matter of great concern. The rapid pace of growth in sickle cell in different tribal populations of India as revealed in the current survey (Table: 1) suggest an urgent need for systematic survey, screening and overall awareness impact assessment among the carriers. The study refers to the international method (source: Cecilia Maryann Rajakaruna, University of Pittsburgh, 2009) for accessing awareness impact in systematic stages through repeated visit to the carriers (AS) and their families. In the first table a comprehensive list of awareness education has been defined to educate the individual about the disease and its consequences in individuals and their families .In most of the cases the awareness education never reaches the people as revealed from gradual increase in the frequency of the Sickle Cell anemia cases in different population of Central India and is largely because the lack of awareness review. Therefore, in the current study, a series of suggestions in tabular form (Table 3, 4, 5, 6, 7, 8) have been given to explore the result of knowledge gain from pre questionnaires, post questionnaires and three months follow-up questionnaires method. Never the less, an attempt has been made to introduce the method to evaluate “concern results” of awareness campaign covering pre-questionnaires, post-questionnaires and three months follow up questionnaires.
Discussion
The study reveals that the incidences of sickle cell anemia at neck and corner of India is growing at a rapid pace. This is indeed a growing trend as compared to many developed countries of the world. Understanding about sickle cell anemia, its pattern of inheritance and gravity of multiple problems are well understood and efforts are on to minimize the load of genetic endowment of sickle cell anemia through wide range of screening and medical aids as per necessity but the trend appears to the reverse(table:1).
Table 1 Growing trend of Sickle Cell Anemia in few tribal populations of Central India
Sl. No |
Community |
Place |
Incidence (%) |
Reference & Year |
1. |
Bhil |
Maharashtra |
18.57% |
Banker et.al., 1984 |
|
Bhil |
Maharashtra |
20% |
Warade, 2007-2009 |
2. |
Gond |
Raipur |
7.96% |
ICMR,1986 |
|
Gond |
Raipur |
7.96% |
Monhanty et al. 1998 |
|
Gond |
Raipur |
17.96% |
Kour et. al., 2013 |
3. |
Korku |
|
9.96% |
Monhanty et al. 1998 |
|
Korku |
Amravati district, Maharashtra |
10% |
Kate et. al.,2002 |
4. |
Madia |
Gadchiroli district, Maharashtra |
20.8% |
Lubin et.al.,1973 |
|
Madia |
Gadchiroli district, Maharashtra |
20-35% |
Warade, 2007-2009 |
5. |
Otkar |
Gadchiroli district, Maharashtra |
35% |
Lubin et.al.,1973 |
|
Otkar |
Gadchiroli district, Maharashtra |
35% |
Warade, 2007-2009 |
6. |
Paware |
Maharashtra |
17.80% |
Banker et.al., 1984 |
|
Paware |
Maharashtra |
20% |
Warade, 2007-2009 |
7. |
Pradhan |
Maharashtra |
33.50% |
Banker et.al., 1984 |
|
Pradhan |
Maharashtra |
20-35% |
Warade, 2007-2009 |
As a student of anthropology, it is our ardent duty to look into the problem from the view point of its distribution and variation in population through time and space. The current endeavors directed to ascertain the awareness impact of this genetic disorder among the people at large and community in particular. The study reveals that, certain identified tribal population with high incidences of sickle cell anemia in Central India (table1) shows steady growth of this genetic disorder during last few decades and reason of this growing incidence is largely because of lack of awareness and impact analysis.
Here, the main emphasize has been given to promote reasonable access to the health services in community sector. Access to scientific and technical support of the areas for the prevention and management of the sickle cell anemia. And last but most important things is to promote and encourage and support impact research work to improve quality of life for those affected. It has been seen that between 19-30 years age individuals are having lack of basic understanding of the sickle cell anemia21.So the current study is an initiative to educate students from their schooling stage or teen-age period where they can have basic knowledge and awareness about the nature and extent of sickle cell anemia. So, the purpose of the study is to spread awareness among the people of tribal areas who are at the risk of having this hemoglobin disorder and repeatedly undergo treatment. In these regards a western reference about American Black and Hispanic American have been given where in a distinct decrease in frequency of Sickle cell disease has been noted in one decade i.e. 2001 to 2011 (table:2). Prevalence levels of SSD decreases to between 1% to 2% in North Africa and to less than 1% in South Africa. In countries like Cameroon republic of Congo, Gabon, Ghana and Nigeria, the prevalence is 20% and 30%. While; in some parts of Uganda it is as high as 45%. The information generally should be disseminated and used as evidence to policy making as well as day to day decision making.
The incidences of gradual fall in occurrence of both sickle cell disease (SS) and carriers (AS) in USA as highlight in the tables (table 2A & 2B) are quite interesting. The awareness impact analysis reveals a positive trend to eliminate the heterozygotes from population in due course.
Table 2A Prevalence of Sickle cell disease in USA during 2001
Population |
Year |
SS |
AS |
Black or African American Black |
2001 |
1:13 |
2:13 |
African American Blacks |
2001 |
3:365 |
5:365 |
American birth |
2001 |
1:16,300 |
3:16,300 |
Table 2B Post awareness and surveillance result (2011)
Population |
Year |
SS |
AS |
African Black |
2011 |
1:10 |
1:13 |
African American Blacks |
2011 |
2:365 |
4:365 |
American birth |
2011 |
1:16,300 |
1:16,300 |
However, to some extent this is subject to the migration history of the population at large as in another study the incidences of hemoglobin disorder like Sickle cell anemia, Thalassemia have gained an increasing trend during last decades due to huge influx of population in United Kingdom from other countries specially from Mediterranean. Therefore, apart from the available record the events of demographic changes due to influx of population, migration and selective factors are to be considers
Conclusion
The current study has been framed under the Anthropological perspective based on integrated method to make it more relevant to the model “Survival and Wellbeing” 10 and thus an attempt to reduce the load of genetic endowment to Sickle cell disease in different population. The original model (awareness development) has been universally accepted and yielded very good result as shown among the American Blacks and American Hispanic births. If it is reinforced in a systematic, equitable and effective manner, through integrated program comprising surveillance, dissemination of knowledge, awareness response, counseling under a specific socio-economic condition in different tribal areas of India, a positive health and wellness response would definitely be achieved.
Acknowledgement
The author acknowledges the academic support by Prof. Subir Biswas, West Bengal State University. I also acknowledge the help of Dr. P Gangopadhay, Course coordinator Anthropology, Indira Gandhi National Open University, Nagpur for necessary advice as and when required.
References:
1.Bain Barbara J. (2006), Haemoglobinopathy Diagnosis, Wiley-Blackwell.
2.Balgir R. (2007), Epidemiology, Population Health Genetics and Phenotypic Diversity of Sickle Cell Disease in India, The Internet Journal of Biological Anthropology, 1(2).
3.Bhatia H.M.& Rao V.R (1986), Genetic atlas of the Indian tribes, Mumbai: Institute of Immunohaematology,19.
4.Cassie Jessica Osbourne (2011), Sickle Cell Disease Awareness amongst College Students, University of Illinois at Urbana-Champaign.
5.Chirag Desai, Krunal Bhandari, Dr. Atul M Desai, Dr. Brien Shah (2014), Awareness on Sickle Cell Anemia in Higher Secondary School Students of Tribal Area: An Initiative, JPSBR;4(6).
6.Das M.K., Singh S.S., Adak T., Vasanth K., Mohanty D. (2005), The Duffy blood groups of Jarawa’s - the primitive and vanishing tribe of Andaman and Nicobar Islands of India. Transfus Med, 15.
7.Deore A. U. & Zade S. B (2013), Epidemiology of sickle cell disorder: The urban scenario in Maharashtra, India, International Journal of Public Health and Epidemiology,2(5).
8.Dr. R. B. Gupta, (2003), Sickle Cell Disease Load in Madhya Pradesh, Regional Medical Research Centre for Tribal, Jabalpur,3(1).
9.Epstein Charles J. Childs B, Clarke FF, McKusick VA, Miller JR, Motulsky AG, et al. (1975), Genetic Counselin, Am J Hum Genet 27: 240-2.
10.Gangopadhay S. & Gangopadhay P. (2013), Model for impact assessment of awareness programme in Sickle Cell Anemia- Development initiative for survival and wellbeing, Journal of Anthropological Survey of India,61(2) & 62(1).
11.Gajpati District in South Orissa, Indian Journal of Community Medicine,28 (4).
12.Ghai O.P., Essential Paediatrics, New Delhi, Interprint, 5th Edn., pp. 100.
13.Kate S.L.& Lingojwar D.P. (2002) Epidemiology of Sickle Cell Disorder in the state of Maharashtra. Indian J Hum Gene, 2(3).
14.Kar B.C. (1991), Sickle cell disease in India, J AssocPhysicians India,39(12).
15.Kaur M. Dangi CBS ,Singh M, Singh H, Kapoor S. (2013), BURDEN OF SICKLE CELL DISEASES AMONG TRIBES OF INDIA- A BURNING PROBLEM, International Research Journal of Pharmaceutical and Applied Sciences (IRJPAS),3(1).
16.Kaushika Rautray, Sourya Acharya, Samarth Shukla, Neema Acharya(2016) Aawareness On Sickle Cell Disease (SCD) And Prevention Of Sickle Cell Crisis In Patients Of Sickle Cell Anemia. A Questionnaire Based Study,International Journal Of Medical Science And Clinical Inventions,3(2).
17.Lehmann H, Cutbush M. (1952),Sickle cell trait in Southern India, British Medical Journal,1(1).
18.Mohanty Dipika & Das Kishalaya(2011), Genetic counseling in tribals in India, Indian Journal of Medical Research,134.
19.Murhekar K.M., Murhekar M.V.(2004), Absence of Haemoglobinopathies and G6PD deficiency among the Jarawas, a primitive Negretoid tribes of Andaman and Nicobar Islands, Indian J Hum Genet,10(1).
20.Office of Registrar General, India. The data of scheduled tribes of Maharashtra. The Census of India; 2001. Available at: cenusindia.gov.in/SCST/dh_st_maha.pdf. Accessed on March 13th, 2013
21.Ogamdi S.(1994), African-American students awareness of sickle cell disease, Journal of American College,43(5).
22.Pande P.L., Singh MPSS, Tiwary R.S(1999), Distribution of ABO and Rh blood groups among the Kodku tribe of Sarguja district, Madhya Pradesh, J Hum Ecol,10(5-6).
23.Rahimi Z., Karimi M., Haghshenass M., & Merat A.(2003) β‐Globin gene cluster haplotypes in sickle cell patients from southwest Iran, Am J Hematol,74(3).
24.Reports of the tribal studies in Jhabua, Ratlam,Ambikapur, Raipur districts of Madhya Pradesh,Ranchi district of Bihar(1986), Institute ofImmunohematology (ICMR),Bombay.
25.Roshan B. Colah, Malay B. Mukherjee, Snehal Martin & Kanjaksha Ghosh(2015),Sickle cell disease in tribal populations in India, National Institue of Immunohaematology (ICMR), Mumbai, India.141
26.Reddy P.H., Petrou M., Reddy P.A., Tiwary R.S., Modell B.(1995), Hereditary anaemias and iron deficiency in a tribal population (the Baiga) of central India, Eur J Haematol, 55(2).
27.Sahu T, Sahani N.C., Das S, Sahu S.K.(2003) , Sickle Cell Anemia in Tribal Children of Shukla R.M., Solanki B.R.(1958), Sickle cell trait in India. Lancet, 1(7015)
28.Sickle Cell Anemia Control Project - Health and Family Welfare .www.gujhealth.gov.in/.../1_sicklecell-anemia-control-programme.
29.ShuklaR.N.,SolankiB.R.(1958)Sickle-Cell Trait in Central India.ISSUE,271(7015).
30.Warade J., Pandey A.(2014)Distribution of Sickle Cell Disease in Different Communities of Patient Visiting Out Patient Department. J Pharm Biomed Sci . 04(08).
31.Winters C.A.(2007), Did the Dravidian Speakers Originate in Africa? BioEssays. 27(5).
32.Winters A.(2008), Origin and spread of Dravidian speakers, International Journal of HumanGenetics,8(4).
33.ssWinters C.(2011),Sickle Cell Anemia In India And Africa,The Internet Journal of Hematology,7 (2).
Barnali Chakraborty, Department of Anthropology, West Bengal State University, North 24 Parganas, West Bengal, India, E-mail: barnalichakraborty999@gmail.com
Arup Majumder, School of Languages and Linguistics, Jadavpur University, Kolkata- 700032
E-mail:arup2make@yahoo.com
Back to Home Page
Frontier
Aug 8, 2020
Arup Majumder arup2make@yahoo.com
Your Comment if any
|
